Research article | Published November 6, 2022 | Original research published in Neurotherapeutics
Multiple Sclerosis: What We Can Learn Even from Failed Approaches to Antibody Therapies
Yasmin Aghajan
is a Clinical Fellow in Neurology at the Department of Neurology, Massachusetts General Hospital, Boston (profile).
Original research: Krämer, J., Wiendl, H. What Have Failed, Interrupted, and Withdrawn Antibody Therapies in Multiple Sclerosis Taught Us?. Neurotherapeutics 19, 785–807 (2022). https://doi.org/10.1007/s13311-022-01246-3
Subjects: Clinical trials, Drug development, Monoclonal antibodies, Antibody therapy, Failure, Multiple sclerosis
New Ground article reviewed by: Julia Krämer and Heinz Wiendl
A recent review, authored by Julia Krämer and Heinz Wiendl and published in Neurotherapeutics, outlines the studies conducted in recent years on various monoclonal antibody therapies for multiple sclerosis (MS). These therapies target various cells and mechanisms that play a role in the development of the neurodegenerative disease: T cells, B cells, cytokines, antivirals, lymphocyte trafficking, and neuroregeneration. Many of the approaches attempt to specifically suppress the body’s immune response, which malfunctions in MS, causing it to attack healthy tissue.
Understanding why certain trials fail can provide valuable insights into how future studies and outcome measures should be designed. Unfortunately, the results of failed studies are not always published. In other cases, the reason for a given study’s discontinuation is not made public, so the authors’ analysis of those trials is necessarily incomplete.
Krämer and Wiendl focused on monoclonal antibody therapies for relapsing-remitting MS and progressive MS that had been trialed in phase II or phase III studies since 2015 and either failed to meet the primary goals, or endpoints, of the study or had to be canceled due to serious adverse events. In some cases, the reasons for the study’s discontinuation were not clearly revealed to the public (while the sponsors stated that safety concerns did not play a role in these cases).
In addition, the review discussed several studies with the antibodies rituximab and natalizumab, which have been approved to treat relapsing-remitting MS. The trials presented were intended to determine whether they can also help treat the progressive form of MS, for which the shortage of immunotherapies is especially serious – but failed to confirm their suitability.
In the following, we highlight the major findings of Krämer’s and Wiendl’s publication.
Approved and later withdrawn: T-cell targeting with daclizumab
Traditionally, MS has been considered a T-cell-mediated autoimmune disease, although a more recent understanding of MS pathophysiology reveals the involvement of nearly all immune cell types. However, T cells are still a crucial player. They are targeted by many of the 18 currently approved disease-modifying therapies, which do not cure MS but can delay disease progression.
In particular, the case of the monoclonal antibody daclizumab is very telling. The antibody blocks the interleukin-2 receptor, which can be found on certain cells of the immune system. As a result, the proliferation of activated T cells is inhibited and the immune regulatory CD56 natural killer cells are stimulated. The latter remove activated CD4+ and CD8+ T cells, thereby reducing the immune response. Moreover, daclizumab reduces the number of lymphoid tissue inducer cells, which also play a role in the pathogenesis of MS. The antibody was originally developed as a therapy to prevent organ rejection in patients with renal transplants. Based on phase II and III trials in 2016, it was also approved for relapsing-remitting MS.
The daclizumab trials were intended to measure differences in the number of MS lesions – areas damaged by the immune system’s response – in the central nervous system. The CHOICE trial evaluated the ability of add-on high and low doses of daclizumab compared to interferon beta alone to reduce the number of new or enlarged lesions in MS patients with active disease. The study showed that add-on high-dose daclizumab reduced the number of new or enlarged lesions compared with the administration of add-on low-dose daclizumab or interferon beta alone.
Subsequently, daclizumab’s chemical structure was modified to reduce cytotoxicity, and it was studied further in SELECT. The new structure was also successful in reducing the annual relapse rate, the mean number of new lesions, and disability progression. SELECTION extended this trial with the same patients for 8 more years, observing a sustained effect on disease activity. Thus, a phase III trial, DECIDE, was conducted in patients with active relapsing-remitting MS. Compared to interferon beta, daclizumab again significantly reduced the relapse rate, number of lesions, and disease progression. EXTEND, too, showed improved outcomes for daclizumab. Based on these trials, the antibody was approved by the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) in 2016.
In the interim, however, serious adverse events have been reported, including infections, skin reactions, and liver abnormalities. In the extension trials, inflammatory syndromes and lymphadenopathy were observed. Serious rashes, such as DRESS and toxic eruptions, developed. There were a few cases of serious liver injury and one case of fatal liver failure due to hepatitis. Increased safety regulations did not solve the problem: subsequently, there were reported cases of autoimmune encephalitis, rheumatological disorders, and further incidences of liver failure. In March 2018, after 12 reports of serious inflammatory brain disorders leading to the death of three patients, daclizumab became the first approved MS biological agent to be subsequently and permanently withdrawn from the market. The authors highlight the difficulty of detecting rare but serious adverse events in phases I to III of trials and the importance of conducting phase IV trials at a time when the substance is already on the market and widely used.
In contrast to these results, daclizumab has shown excellent tolerability and long-term safety in kidney transplant patients, for whom it was initially developed. Arguably, there are marked immunophysiological differences between renal transplant patients and MS patients. Accordingly, blocking the same interleukin-2 receptor may trigger different cytokine signaling pathways in different patient populations.
Highly complex: B-cell targeting with tabalumab, lanalumab and belimumab
B cells also play a central role in the pathophysiology of MS. There is evidence of B cells infiltrating the central nervous system, of abnormal inflammation-promoting cytokine production in B cells, and of increased levels of B-cell-relevant cytokines and chemokines in the cerebrospinal fluid of MS patients. In addition, there have been striking results from B-cell depletion therapies that sought to reduce B-cell lines by administering rituximab, ocrelizumab and ofatumumab. All disease-modifying therapies approved for MS have had some suppressive effect on B cells or modulated their effects on the immune response.
Other substances have proven less effective. The monoclonal antibody tabalumab is a human immunoglobulin G4 that neutralizes the B-cell activating factor BAFF. If not neutralized, BAFF activation leads to T-cell activation and the maturation and survival of B cells. A phase II study, which was completed by nearly 200 patients with relapsing-remitting MS, failed to meet its primary goal: there were no differences in the cumulative number of lesions that were visible in magnetic resonance imaging (MRI) scans after administering a gadolinium-based contrast agent; nor was there any impact on secondary outcomes. Additionally, treatment-related adverse events were more frequent. A trial with lanalumab was terminated very early, based on the sponsor’s strategic considerations. The outcomes, therefore, were not conclusive. Belimumab, which is a drug approved for systemic lupus erythematosus and active lupus nephritis, also underwent a trial for relapsing-remitting MS. However, this study was also terminated prematurely, and its results have not yet been published.
Krämer and Wiendl suggest that tabalumab was not effective, since it had little impact on the inhibition of memory B cells, which are a central player in the immunopathogenesis of MS. This observation was made by another research group in 2020 (see here). Additionally, the authors suspect that the antibody perhaps also preserved T-cell activation. Given that other B-cell targets – such as the antigen anti-CD20 – respond better to treatment, the authors view the overall situation as an indication of the highly complex nature of B-cell actions in MS.
Limited data: Cytokine-directed therapy with secukinumab
Cytokine molecules such as interferons are another major player in the MS disease process. To date, interferon therapy is the only approved cytokine-directed therapy for MS. Attempts have been made to treat MS patients with either anti-inflammatory cytokines or inhibitors of proinflammatory cytokines.
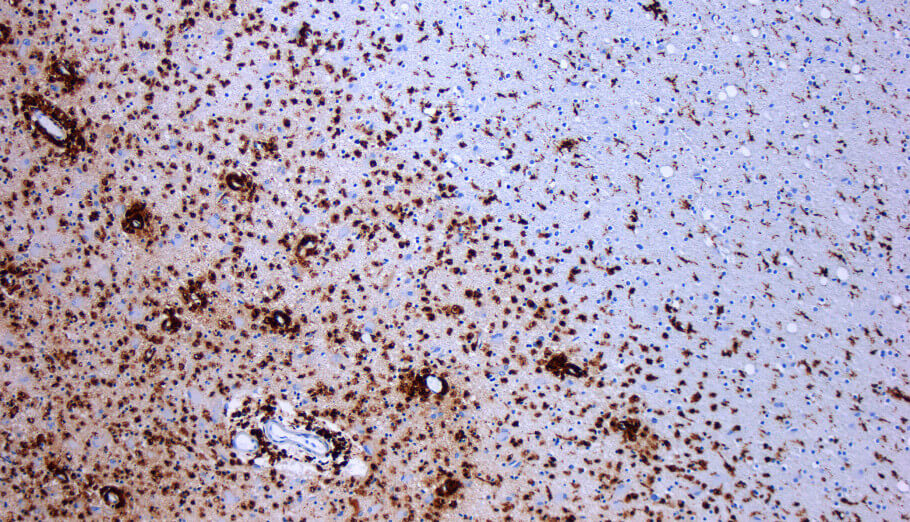
The monoclonal antibody secukinumab, a human immunoglobulin G1k, binds to and neutralizes the cytokine interleukin 17A, which is a potent inducer of inflammation. Interleukin 17A is produced by proinflammatory T helper 17 cells, among others. Increased levels of the former and an increased proportion of the latter have been observed in the brain tissue of MS patients, especially in MS lesions. In addition, both are more frequently detected in the peripheral blood and cerebrospinal fluid of MS patients.
Secukinumab is approved for the treatment of psoriasis, psoriatic arthritis, and ankylosing spondylitis. A few studies investigating the effects of secukinumab on MS were conducted from 2012 to 2014. The initial phase II study failed to reach its primary goal, defined as a reduced number of new gadolinium-enhanced and new or enlarging T2-weighted lesions without double counting, observed in monthly MRI brain scans from week 4 to week 24. However, the treatment did significantly reduce the mean cumulative number of new lesions starting in week 16 through the end of the study in week 36. In week 36, the researchers also observed a significant difference in lesions. The rate of adverse events was similar for the placebo group, although mild to moderate infections were more frequent in the treatment group. In a 12-month extension study, patients continued to receive secukinumab, but the study was discontinued for unknown reasons. A subsequent phase II study was terminated early after only 28 patients had enrolled; this was because a more promising antibody targeting interleukin 17 had since been developed, CJM112. Unfortunately, there have been no relevant studies on the latter to date.
Due to the limited data available, it is difficult to draw conclusions. According to Krämer and Wiendl, imbalances within the study group with regard to disease activity on the basis of MRI scans, but also with regard to sex and age, partially obscured secukinumab’s treatment effect. However, a clear and pronounced therapeutic effect – based on the number of lesions – was observable from week 12 of the study. The authors contend that cytokine-directed therapies are complex by their very nature, since individual cytokines may have diverse and even opposing functions.
Largely ineffective: Antiviral approach with temelimab
There is growing evidence that MS may be triggered by herpesviruses – Epstein-Barr virus, cytomegalovirus, human herpesvirus 6, varicella-zoster virus – and human endogenous retroviruses, as well as by bacterial infections such as chlamydia and Staphylococcus aureus. For example, a study recently published in Science on more than 10 million young adults (see here) indicated exposure to the Epstein-Barr virus as one of the leading triggers of MS.
Consequently, antiviral therapies came into the focus of MS researchers. The pathogenic HERV Type-W envelope protein (pHERV-W ENV) seemed to be a good starting point. In the course of evolution, human endogenous retroviruses (HERVs) became embedded in the genome, but are nearly always inactive or nonfunctional today. However, under certain circumstances, they may cause damage. The pathogenic HERV-W ENV is such a case: it drives immune activation, inflammation, and neurodegeneration in MS and keeps the protective myelin coating around nerve fibers in the central nervous system from regenerating.
The monoclonal antibody temelimab is a recombinant humanized immunoglobulin G4 that works against pHERV-W ENV. However, the currently available studies do not definitively answer the question of whether pHERV-W ENV modulation can affect the development of MS. The phase II trial CHANGE-MS and its extension ANGEL-MS confirmed no significant effects in terms of the number of lesions. At a certain point in the study, at least a trend toward reduced lesions could be observed in patients who had manifested gadolinium-enhanced lesions at baseline at the beginning of the study, and who had received the highest doses of temelimab. Another phase II study, ProTEct-MS, began evaluating patients with prior exposure to rituximab and temelimab but is currently suspended and no longer recruiting patients.
Ended prematurely: Blocking lymphocyte trafficking with vatelizumab
Integrins are members of the family of cell adhesion and signaling proteins that regulate immune cell trafficking between the blood and tissues and are therefore intricately connected to the body’s immune response. One of them is the Α2β1 integrin molecule, also known as the very late antigen VLA-2, which is expressed on many cell types, including lymphocytes. The effect of VLA-2 can be reduced by administering vatelizumab. This is an antibody against VLA-2 on activated lymphocytes and is believed to block the interaction of VLA-2 with collagen fibers that build up at inflammatory sites. Therefore, it prevents inflammatory lesions.
Unfortunately, the vatelizumab phase II trial EMPIRE was discontinued for no clear reason (but reportedly not due to side effects or safety concerns). Among others, EMPIRE could have potentially yielded interesting information on the best point in time to administer the antibody: vatelizumab needs to cross the blood-brain barrier to penetrate into the central nervous system, but can only do so when this barrier is already inflamed and therefore more permeable.
Unanswered questions: Neuroregenerative approach with opicinumab
Opicinumab is an antibody against LINGO-1, a membrane protein expressed on oligodendrocytes in the central nervous system. In brain diseases or brain injury, the protein is formed more frequently. Inhibition of LINGO-1 produces beneficial effects, at least in animal studies: it helps both axons and neurons to regenerate, while also allowing the former to remyelinate.
Three phase II opicinumab trials have been conducted for MS patients. The RENEW study evaluated patients with a first episode of unilateral optic neuritis. This inflammation of the optic nerve destroys myelin sheaths and can indicate a risk of developing MS. The patients were given opicinumab following standard treatment with methylprednisolone. To assess the results, the RENEW researchers triggered neuronal activity in the patient’s optic nerve by presenting them visual stimuli. Their subsequent measurements showed significantly improved conduction latency values in the nerve. In another phase II trial, SYNERGY, patients with relapsing-remitting MS and secondary progressive MS received varying doses of opicinumab in addition to interferon beta. The study measured confirmed disability improvement, a quantitative method used to assess disabilities in patients. There was weak evidence of improvement with a smaller dose and some improvement with a higher dose, but not for as many patients as expected. The third and last phase II trial was AFFINITY, which involved the treatment of patients with relapsing-remitting MS and secondary progressive MS with opicinumab as an add-on to interferon beta, dimethyl fumarate, or natalizumab. Biogen, the study’s sponsor, discontinued the trial in 2020, since its goals had not been met.
Is neuroregeneration, or more specifically, remyelination, a clinically relevant therapeutic strategy for MS? While opicinumab leads to remyelination in animals, Krämer and Wiendl – in line with other groups that questioned this point – still feel it is unclear whether the antibody truly crosses the human blood-brain barrier and reaches the central nervous system. To date, it also remains unclear what the ideal time to initiate remyelination therapy is, and what the ideal outcome for proof of concept would be.
Failed attempt: Treatment of progressive MS with antibodies approved for relapsing-remitting MS
Natalizumab
Natalizumab is a humanized monoclonal antibody against α4-integrin (VLA-4), which is expressed on leukocytes. It hinders B and T cells, macrophages, and dendritic cells from migrating into the central nervous system, thereby decreasing the activation of microglial cells in the brain, which may reduce inflammation. The antibody is approved and highly efficacious in the treatment of relapsing-remitting MS. In 2016, the phase III ASCEND trial sought to determine whether similar effects could be achieved in the treatment of secondary progressive MS. Several clinical scores were used to measure clinical disease progression, but no significant effects were observed; only some disability progression of the upper limbs was shown to be reduced.
The authors suggest possible reasons for natalizumab’s failure when used to treat secondary progressive MS. In relapsing forms of the disease, for which it was developed, leukocyte “outside-in” traffic into the central nervous system plays the biggest role, while progressive MS seems to be independent of this process. They suggest considering progressive MS as more of a “compartmentalized inflammation” that is to some extent decoupled from leukocyte traffic and other processes in the immune system. It is also clear that natalizumab does not cross the blood-brain barrier well.
Additionally, the authors question whether the clinical scores always captured all relevant aspects of disability. Generally, the Expanded Disability Status Scale (EDSS) is used to measure disability progression in patients with progressive MS; on this scale, higher values indicate a higher disability. But lower EDSS rates suffer from high variability between the assessments made by different raters, and higher EDSS rates greatly depend on walking ability. Therefore, changes in disability may not be adequately detected or reflected.
Increasing the length of follow-up phases, the authors suggest, might therefore improve the detection rate and help to reveal treatment effects. More generally speaking, future studies will have to identify which outcome measures might be more suitable to identify changes in patients’ disabilities.
Rituximab
The monoclonal antibody rituximab is a mouse-human chimeric against the antigen CD20 on B cells. It was first approved for B-cell non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis, granulomatosis with polyangiitis, and more. Its off-label use for MS, however, is widespread in several countries outside the United States.
Several trials have evaluated rituximab for MS, including a phase II HERMES trial that significantly reduced the number of lesions and the percentage of patients with relapse up to week 24 of the study. On the other hand, the phase II/III study OLYMPUS did not find a significant reduction in disability progression in MS patients with the progressive form of the disease. However, other study goals were reached, including reduction of lesion volume and reduced disease worsening as measured on several scales. Other small phase II studies with rituximab include STRIX-MS, RIVITaLISe, GATEWAYII and EFFRITE.
Despite some promising results, the clinical development of rituximab was interrupted when anti-CD20 antibodies such as ocrelizumab, which are next-generation monoclonal antibodies but follow the same principles, entered the scene. Ocrelizumab is less immunogenic and triggers fewer anti-drug antibodies, thus resulting in a better safety profile and efficacy. In addition, the patent on rituximab has since expired; accordingly, the pharmaceutical industry has little interest in further research.
While rituximab failed to treat progressive MS, it is effective in treating relapsing-remitting MS and is commonly used around the globe with good effects and good safety profiles. A lower-cost biosimilar that has also been approved will further increase its use, the authors assume.
Conclusion: Dealing with shortcomings and missing data
Since 2015, quite a number of monoclonal antibodies have failed to succeed in studies for relapsing-remitting and progressive MS. Among others, the story of daclizumab, an anti-T-cell drug that is approved in renal transplant patients but failed to treat MS, shows the importance of detecting rare adverse events in a pharmacovigilance setting after approval, including phase IV studies. It also shows that antibodies that are safe for other autoimmune conditions may not have the same safety profile in MS patients due to differences in immunopathogenesis. In turn, tabalumab’s story illustrates the importance of B memory cells in MS pathology.
However, several attempts to use drugs targeting other mechanisms of action, such as cytokine modulation and antiviral and neuroregenerative therapies, haven’t yielded convincing results. Drugs that are effective in relapsing-remitting MS, such as natalizumab, may not necessarily work in progressive MS due to the differences in their pathophysiologies, mainly marked by the more compartmentalized biology of the central nervous system in the case of progressive MS. There also seems to be a need for future antibodies targeting progressive MS to more successfully cross the blood-brain barrier.
Thanks to the many trials that have been conducted, the knowledge database available to researchers in terms of understanding MS pathology and clinical trials is growing steadily. Nevertheless, Krämer and Wiendl consider MS research to be lacking. Learning from trials in which monoclonal antibodies failed, or from those that were discontinued, is only possible if their results are published. This is indispensable, Krämer and Wiendl argue, as otherwise precious information may be lost, no matter if the trial in question was a “hit” or a “miss.”
How to reuse
The CC BY 4.0 license requires re-users to give due credit to the creator. It allows re-users to distribute, remix, adapt, and build upon the material in any medium or format, even for commercial purposes.
You can reuse an article (e.g. by copying it to your news site) by adding the following line:
Multiple Sclerosis: What We Can Learn Even from Failed Approaches to Antibody Therapies © 2022 by Yasmin Aghajan is licensed under Attribution 4.0 International
Or by simply adding:
Article © 2022 by Yasmin Aghajan / CC BY
To learn more about the available options, and for details, please consult New Ground’s How to reuse section.
This article – but not the graphics or images – is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/.
This article – but not the graphics or images – is licensed under a Creative Commons Attribution 4.0 License.
